Hernia Surgery Research Study
Hernia Surgery Research Study
Jean Brown
1/1/20251 min read
Hernia Surgery Research Study
Are you planning on having an inguinal hernia repaired?
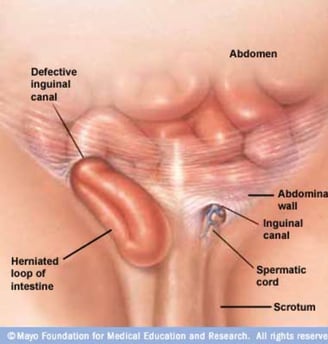
Jean Brown Research is conducting a clinical research study for an investigational pain relief implant.Participants that qualify for the study may receive surgery, study-related care and pain relief implant at no cost to them. Qualified participants may also be compensated for their time and travel. Basic qualifications are: Ages 18 and older Male or Female Generally in good health Be eligible for unilateral inguinal (groin) hernioplasty with mesh. (Repair of multiple hernia through a single incision is permitted). If you qualify you may receive: No cost hernia repair Study-related care Investigational pain relief implant You also may be compensated for your time and travel related to the study. To see if you qualify, please complete and submit your information or call 801-261-2000. What is an Inguinal Hernia? An inguinal hernia is more common in men and usually occurs in the inguinal canal in the groin where the spermatic cord enters the scrotum. In women, the inguinal canal is where the ligament attaches to the uterus. What causes an Inguinal Hernia? An inguinal hernia occurs when soft tissue–usually part of the membrane lining the abdominal cavity (omentum) or part of the intestine–protrudes through a weak point in the abdominal muscles. When pressure is exerted in the abdomen, it increases pressure on the weak spot and can be painful. The pressure and resulting pain may be caused by: Straining during bowel movements Strenuous physical activity like lifting something heavy Chronic cough or sneezing Pregnancy Ascites (Fluid build-up in the abdomen) Aging Hernia Treatment Options Not all hernias need immediate surgery, but if you are experiencing pain or your hernia is growing, you may need hernia surgery. Hernias can be repaired surgically or laparoscopically.

Care
Expert surgeons providing personalized hernia treatment options.
Trust
Health
info@herniascentre.com
Tel: 01473279123
© 2025. All rights reserved.
Among patients undergoing incisional hernia repair, the use of mesh to reinforce the repair was associated with a lower risk of hernia recurrence over 5 years compared with when mesh was not used. However, with long-term follow-up, the benefits attributable to mesh were offset in part by mesh-related complications, according to a study published online by JAMA. The study is being released to coincide with its presentation at the American College of Surgeons Clinical Congress 2016.
Elective incisional hernia repair is one of the most commonly performed general surgical operations. In the United States alone, about 190,000 inpatient abdominal wall hernia repairs were performed in 2012. Prosthetic mesh is frequently used to reinforce the repair; it'susede in at least half of the abdominal wall hernia repairs performed in the United States. The benefits of mesh for reducing the risk of hernia recurrence or the long-term risks of mesh-related complications are not known.
Dunja Kokotovic, M.B., and Frederik Helgstrand, M.D., D.M.Sc., of Zealand University Hospital, Køge, Denmark, and Thue Bisgaard, M.D., D.M.Sc., of Hvidovre Hospital, Hvidovre, Denmark, conducted a study that included 3,242 patients with elective incisional hernia repairs in Denmark from January 2007 to December 2010. The researchers compared outcomes for hernia repair using mesh performed by either open or laparoscopic techniques vs open repair without the use of mesh.
Among the patients (average age, 59 years; 53 percent women), 1,119 underwent open mesh repair (35 percent), 366 had open nonmesh repair (11 percent), and 1,757 had laparoscopic mesh repair (54 percent). The median follow-up after open mesh repair was 59 months; after nonmesh open repair, 62 months; and after laparoscopic mesh repair, was 61 months. The researchers found that the risk of the need for repair for recurrent hernia following these initial hernia operations was lower for patients with open mesh repair (12 percent; risk difference, -4.8 percent) and for patients with laparoscopic mesh repair (10.6 percent; risk difference, -6.5 percent) compared with nonmesh repair (17.1 percent).
For the entirety of the follow-up duration, there were a progressively increasing number of mesh-related complications (such as bowel obstruction, bowel perforation, bleeding, late abscess) for both open and laparoscopic procedures. At 5 years of follow-up, the cumulative incidence of mesh-related complications was 5.6 percent for patients who underwent open mesh hernia repair and 3.7 percent for patients who underwent laparoscopic mesh repair. The long-term repair-related complication rate for patients with an initial nonmesh repair was 0.8 percent (open nonmesh repair vs open mesh repair: risk difference, 5.3 percent; open nonmesh repair vs laparoscopic mesh repair: risk difference, 3.4 percent).